Series Hosted by Karmanos Cancer Institute’s Office of Community Outreach and Engagement and the Detroit Public Library Continues Through November
The Barbara Ann Karmanos Cancer Institute’s Office of Community Outreach and Engagement (COE) has continued its Community Conversations on Cancer series in 2025 in partnership with the Detroit Public Library. The program invites members of the public to dialogue about current cancer research and treatment, improved health outcomes, and a deep understanding of a cancer diagnosis.
The 2025 series includes six events, each a collaborative, informative discussion introducing the community to a different aspect of modern cancer research and care. The series started in May, discussing cutting-edge breakthroughs in liver cancer treatment. In June and July, the talks focused on lung and prostate cancer diagnosis and treatment.
The fourth Community Conversations on Cancer event in 2025, “Of Mice and Women: Connecting the Dots to Strengthen Uterine Cancer Research,” is set for Sept. 17. The event, presented by Michael Wilson, Ph.D., member of the Molecular Therapeutics (MT) Research Program at Karmanos and assistant professor at Wayne State University School of Medicine’s Department of Oncology, will discuss how he works with a community advisory board (CAB) of four women who help inform and articulate the public relevance of his work. Members of the advisory board will moderate.
Events are also planned in October and November. Each event is open to the public and held at the Detroit Public Library’s Main Branch and virtually via Zoom.
The Latest Breakthroughs
Boris Pasche, M.D., Ph.D., FACP, president and CEO of Karmanos and chair of the Department of Oncology at Wayne State University (WSU) School of Medicine, started the 2025 series on May 28 with a conversation about an exciting cancer treatment innovation he helped develop that is now available at Karmanos. “The Next Breakthrough in Cancer: Treatment with Radiofrequencies” discussed the TheraBionic P1 device, which he was a co-inventor.
The newly FDA-approved device is based on the discovery of tumor-specific radiofrequencies, similar to those used in mobile phone communications, to treat the most common form of liver cancer, hepatocellular carcinoma (HCC). He spoke about how the idea for the device was developed and how it works.
“We modulated this signal with very precise devices, and we measured the pulse of these patients with cancer,” he said. “To our surprise, we found that patients with the same type of cancer were always experiencing changes in pulses at the same frequencies.”
After decades of research, this discovery led to the development of the TheraBionic P1 device. Pasche and his team found that many tumors responded to specifically tuned radiofrequencies, and either stopped growing or shrank in patients undergoing this therapy.
The TheraBionic P1, though recently approved for HCC, has been under study for over 20 years. In those studies, patients reported none of the debilitating side effects, like gastrointestinal distress or loss of appetite, associated with other cancer-fighting therapies. Overall, studies showed treatment efficacy, minimal adverse side effects, symptomatic benefit, and convenience of treatment. Patients with HCC saw a 34% increase in survival rates using the TheraBionic P1. In patients with advanced HCC, 50% reported their disease had stabilized for six or more months, and 10% reported tumor shrinkage.
Treatment with the TheraBionic P1 is currently available for adult patients with advanced hepatocellular carcinoma who have failed first- and second-line therapies. It is currently approved for HCC, though the work of Dr. Pasche and his team has identified radiofrequencies specific to several other types of cancer, offering hope that its efficacy is not limited to liver cancer. Dr. Pasche’s team and lead investigators at Karmanos continue to study and develop this promising technology.

Rosalind Sample, Wilma Stringer and Bill Winkler moderated the event. Sample serves as the community outreach coordinator for the Pink Fund, which helps ease the financial burden of patients undergoing breast cancer treatment. It provides housing, transportation and insurance help to patients. Stringer is a division coordinator for development with the Healthier Black Elders Center (HBEC). Winkler has been involved in the Karmanos Cancer Advocacy Program (KCAP), which trains survivors and family members to help direct Karmanos research, and the Patient and Family Advisory Council (PFAC), a group of current and former patients and caregivers who work to improve quality of care and the patient experience.
"I have been associated with Karmanos since 2011, when Karmanos saved my daughter's life,” Winkler told the crowd. “Since then, I have been slowly becoming more deeply involved with what Karmanos does in the community with cancer prevention, detection and cure."
Moderators like Winkler said that the community can benefit from events like these, where they can engage in frank dialogue with front-line doctors and researchers.
"We want to educate as many people as possible,” Winkler added.
“I see educating people as not only educating them in terms of their ability to understand what this research is about, how it works, but also helping people to get beyond the fear, anxiety and impediment to going to have a test — a proactive attempt on the part of people to make sure that they're in good health.”
Moderators at this event and other Community Conversation on Cancer events take that educational role seriously, ensuring the community attending gets the most from the conversation.
“I think the information is delivered well because it’s in layman's terms,” Sample said. “If you don't understand something, you can ask a question immediately.”
Engaging the Public on the Latest Lung Cancer Research
On June 25, Ammar Sukari, M.D., medical oncologist, member of the Thoracic Oncology Multidisciplinary Team (MDT) and the MT Research Program at Karmanos, and associate professor at the Wayne State University School of Medicine, presented “The Road Ahead: Understanding a Lung Cancer Diagnosis and Exploring Treatment.”
Dr. Sukari focused on what to expect following a lung cancer diagnosis and determining the best treatments. He described the types of treatments currently being studied and how these newer treatments compare to the standard of care.
“New medications that come to treat cancer, in general, we always try them first in the advanced stage, like stage four, and then they make their way down to the earlier stages,” Dr. Sukari explained to the audience.
“For example, take EGFR mutations in lung cancer. We have a drug called Erlotinib that was introduced in 2005 and 2006. It was a breakthrough. For people who had that mutation, they had great responses. Later on, we had similar drugs, but more effective. Now, we find that we can use those drugs after surgery for stage I and stage II, and patients will have much better outcomes and less relapse.”
Lung cancer is one of the most common types of cancer. The American Cancer Society (ACS) estimates that there will be over 226,000 new cases of lung cancer in the U.S. in 2025. The Centers for Disease Control and Prevention adds that nearly 50% of lung cancers are also detected at a late stage, complicating treatment and survivorship rates.
Dr. Sukari told the audience about screening tools, like low-dose CT scans, which help at-risk patients and caregivers identify cancers earlier and improve survivor health outcomes. Higher screening rates, Dr. Sukari explained, are good, but he emphasized that he recommended screening only for high-risk groups, like former and current smokers.
Ultimately, he said that, while non-smokers can (and do) get lung cancer, the best way to minimize your risk of lung cancer is not to smoke, and if you do, kick the habit.
“Lungs are designed for air,” Dr. Sukari said, adding that anything other than air — from vape mist to cigarette or hookah smoke — can lead to unhealthy outcomes.
He also spoke to the crowd about newly approved treatments, like immunotherapy, that researchers have studied and seen success with — both in and outside clinical trials.

Jim Scott, Katrina Studvent and Patrick Yankee, COE partners and community leaders, moderated the June event. Scott is active in the Cancer Action Councils (CACs) that COE supports. CAC groups invite survivors, caregivers and advocates into the cancer research process, giving them a strong, community-centered voice in health outcomes. Studvent runs BLARE Together, a non-profit offering programming, navigational support and advocacy for individuals and caregivers impacted by chronic illness and disease. Yankee serves as chief development officer at Corktown Health, which offers primary care, cancer screening, health insurance navigation, and more.
For her part, Studvent said she hopes events like these inspire people to action.
“Take it a step further,” she urged. “If you're within the age bracket of your initial screening for a specific type of cancer, we want to follow up with you and make sure you get that screening. If you have loved ones or family members within this age bracket, let us know how we can support you and help you navigate the resources needed to support those family members. If you've already been diagnosed, let us connect you with someone who can support you along your journey. Just make sure you have those action steps.”
A Public Dialogue on Prostate Cancer
For the third event in the series, Frank Cackowski, M.D., Ph.D., medical oncologist, member of the Genitourinary Oncology MDT and the MT Research Program at Karmanos, and assistant professor at the Wayne State University School of Medicine, welcomed the public to his talk, “The Road Ahead: Understanding a Prostate Cancer Diagnosis and Exploring Treatment” on July 23.
Dr. Cackowski’s talk began with what patients and their families might need when facing a new diagnosis. He described the types of treatments currently available and what new patients can expect on their own survivorship path.
“What is the prostate?” Dr. Cackowski rhetorically asked the crowd. “Probably not everybody knows, so we’ll start there. The prostate is a gland whose normal function is to secrete nutrients into the seminal fluid. It’s part of the male reproductive tract. It's right at the bottom of the bladder and surrounds the urethra. That’s important both for diagnosing prostate cancer and the symptoms that it might cause.”
He talked to the crowd about how common prostate cancer is.
“Something like one in six men will get prostate cancer. Not all those cases are severe and aggressive, and not all need to be treated. Sometimes, we can get by with observing. But prostate cancer is very common.”
According to ACS, new diagnoses of prostate cancer in 2025 will exceed 300,000 in the U.S., and more than 35,000 men will die of the disease.
“So, who gets prostate cancer?” Dr. Cackowski continued. “Men, of course. Usually older men. You hardly see it in somebody in their 30s, and usually not in their 40s… The peak age for diagnosis is in the 60s.”
“With screening, prostate cancer tends to be discovered six to 13 years earlier,” he added. “So that kind of gives you some idea about how long it takes to present itself otherwise.”
Earlier detection can make a big difference in how doctors help a patient fight cancer, and how effective that fight may be.
Screening usually involves a blood test called a prostate-specific antigen (PSA) test, a rectal exam, or both.
“It’s a protein,” Dr. Cackowski explained. “It’s made and secreted by the prostate and prostate cancer. All men who have a prostate are going to have some amount of PSA. But if the levels of PSA get higher, then the risk of prostate cancer being there is greater.”
PSA tests have helped doctors find cancers earlier and increased survival rates for prostate cancer patients. The blood tests supplement the digital rectal exam, a reliable and accurate detection technique.
Like most cancer screenings, prostate cancer screening itself carries low risks for patients. However, follow-ups — like MRIs or biopsies — can have slightly higher risk factors, so experts recommend screening only for people within certain guidelines.
In the case of prostate cancer, Dr. Cackowski recommended that men start screening in their late 40s — earlier for some higher-risk groups, like African American men — and continue through age 70. For men below 50 or older than 70, he advised consulting a doctor about whether screening is necessary. Like any medical procedure, patients need to weigh the benefits and risks, particularly those in high-risk groups, and make an informed decision.
“Overall, we want to screen people likely to benefit from the screening,” Dr. Cackowski said.
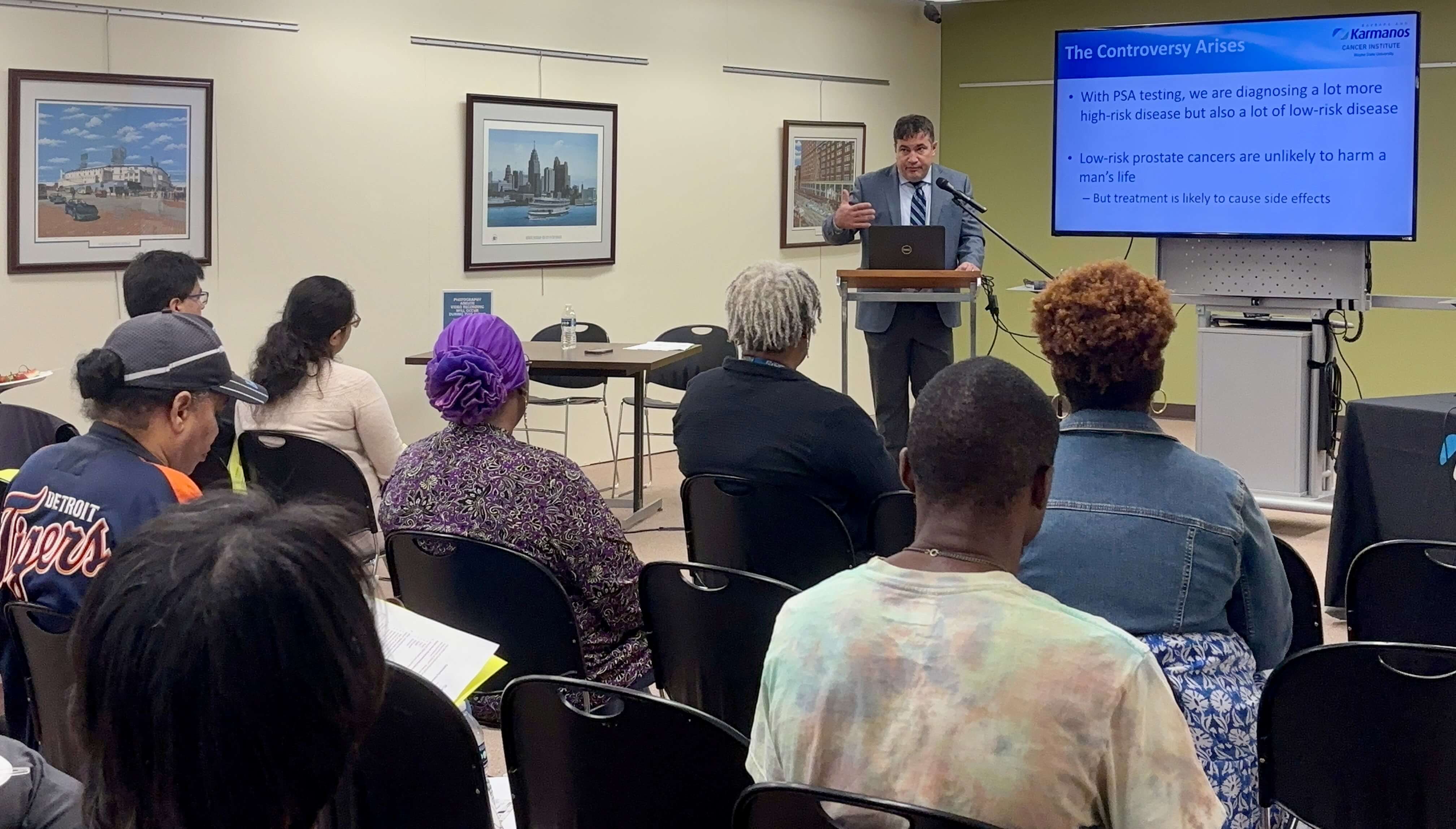
The July event was moderated by Stephen Dewitt, Lossie Pearson and Lance Woods, all community leaders and COE partners. Dewitt works with KCAP. Pearson serves as a lay health advisor with COE. Woods is co-founder of WERUN313. Moderators took questions for Dr. Cackowski from the dozens of people attending in person and dozens more attending virtually via Zoom.
“This topic, in particular, is very near and dear to my heart because this cancer has plagued my family for generations,” Woods said. Two members of Woods’ family directly impacted by prostate cancer attended the event virtually and participated in the question-and-answer session at the end.
Keeping the Conversations on Cancer Going
The Office of Community Outreach and Engagement (COE) fostered these conversations with the collaboration and support of many partners throughout the community, including:
- Cancer Thrivers Network for Jewish Women
- Corktown Health
- Healthier Black Elders Center
- Michigan Ovarian Cancer Alliance (MIOCA)
- National Council of Negro Women, Inc. (NCNW) -- Detroit Section
- New Day Foundation
- The Pink Fund
- WERUN313
- Western Wayne Family Health Centers
These important partners hosted informational tables at the events to engage with the community, raise awareness, and discuss missions and services, and will return for upcoming events.
This year’s Community Conversations on Cancer series continues with three more events:
Sample has attended and moderated and said that any person with a tie to cancer — patient, caregiver, family — can benefit from attending one of the remaining events.
“It gives our community members a place for their voices to be heard and to get those questions answered that maybe they couldn't get answered at their doctor's office. In this community setting, they've made it okay to ask questions so that you do not feel afraid or think the doctors are intimidating. They're not, especially when the doctor gives you a presentation and you can engage with that doctor who's a subject matter expert on your cancer.”
The upcoming Community Conversations on Cancer events will be held at 6 p.m. at the Detroit Public Library’s Main Branch, 5201 Woodward Avenue, Detroit, MI 48202. Events are fully accessible and also available via Zoom. Registration is required.
Click here for more information about these upcoming talks and other dialogues between the community and leading cancer researchers.