Author: Sarah Barber
Fear—it’s the first thing Deborah Nutt felt when she was told that the lump she found wasn’t an infected lymphoid; it was squamous cell (neck) cancer.
Diagnosis
Fear—it’s the first thing Deborah Nutt felt when she was told that the lump she found wasn’t an infected lymphoid; it was squamous cell (neck) cancer.
“When I went in for my routine physical, I mentioned a lump I found on my neck. I thought it was just an inflamed lymphoid. I was prescribed an antibiotic, but the lump kept growing. I was referred to an ear, nose and throat physician, Dr. Goebel, and he did a biopsy. When it came back as cancer, everything moved quickly.”
Treatment
Nutt had the lump removed surgically in mid-September and started radiation and chemo treatments at Karmanos Cancer Institute at McLaren Greater Lansing the first week of November.
“I was devastated, but I kept telling myself I could do this. Everyone was telling me I could do this,” said Nutt.
Head and neck cancer can be one of the hardest oncology treatments to go through. Many patients require a gastrostomy tube (g-Tube) to ensure they get proper nutrition during treatments, which means a surgical procedure is needed before treatment can begin.
“Weeks 6 and 7 were hard,” said Nutt. “I lost all taste, the smell of food made me nauseous, my gag reflex was heightened, and I couldn’t swallow medications or food, and it was hard to keep water down. I had to use my g-tube to get nourishment into my body, but I was still losing a lot of weight.”
It was so difficult that Nutt almost gave up. “I was at the end of my treatments, only one more week to go, and I said to my partner, ‘I can’t do this anymore.’” We went to my doctor’s appointment that day to let them know, and the doctor came into my room and said, ‘Debra, you absolutely can do this; you are almost to the finish line.’”
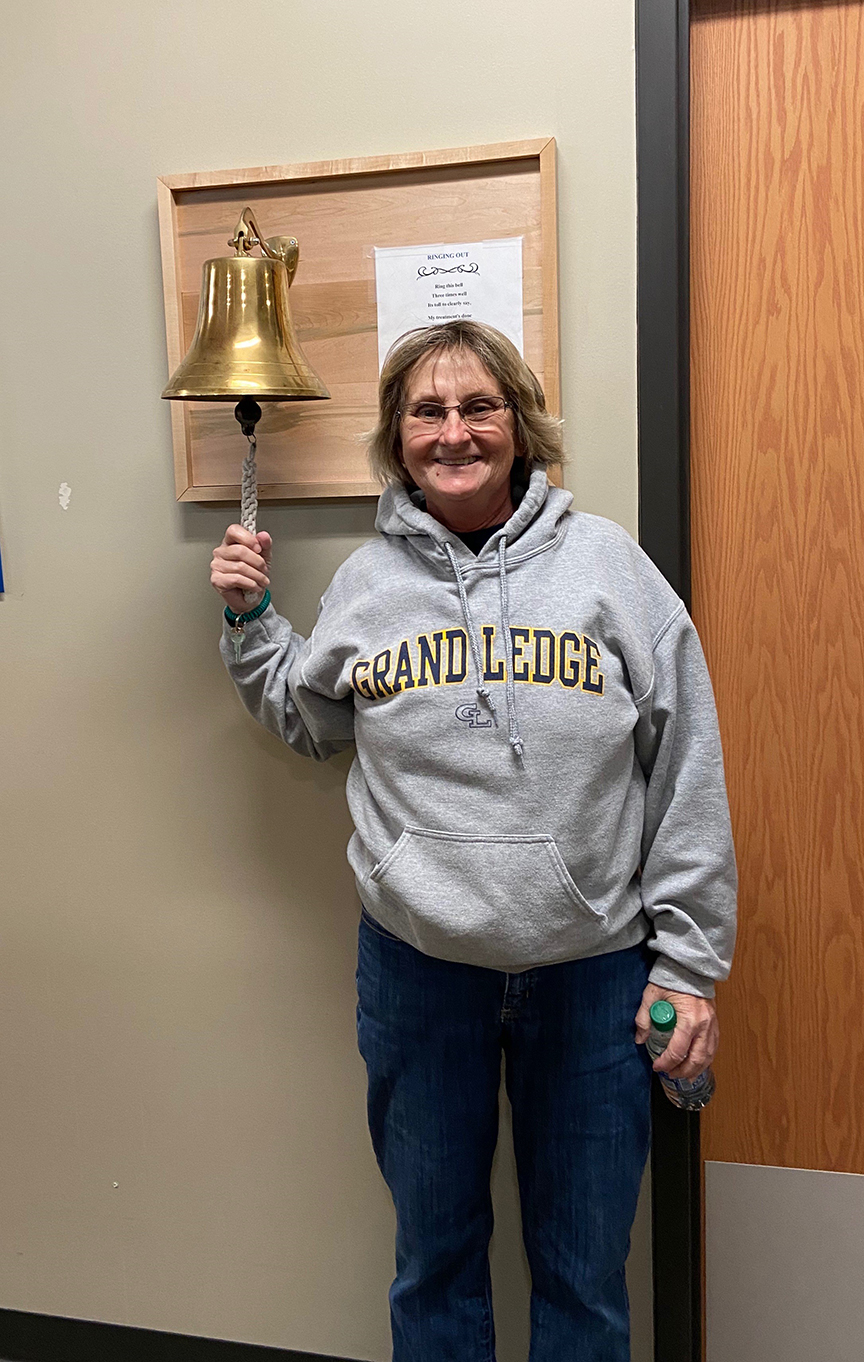
Nutt prayed, envisioned she was out on the golf course and got through the rest of her treatments. On January 6, 2020, at 7:57 a.m., Nutt rang the bell signaling her last treatment day.
Recovery
“It took months for my taste to come back,” said Nutt. “The first thing I was able to taste again was salt, so I started eating salted scrambled eggs.”
Health-related post-traumatic stress disorder (PTSD) can also be a common part of recovery for patients who have gone through a terrifying health experience. It can help to find oncology support or survivor groups that help patients work through fears and concerns related to their oncology journeys.
“I threw out all of the clothes I wore to treatments, and I cut my hair into a different style that didn’t remind me of what I experienced,” said Nutt. “Once you are a survivor, you are always looking over your shoulder.”
However, even though the experience was traumatic, Nutt shared, “Every day that passes I feel a little bit better, and I am glad that I am still here to share my experience with others. I am thankful for my entire team of doctors and nurses, my oncology nurse navigator, and my neighbors, friends, and partner, who took care of me and helped make this experience better. They never gave up on me.”
Learn more about the oncology navigator program at McLaren Greater Lansing by clicking here. For more information about Karmanos Cancer Institute at McLaren Greater Lansing, click here.